Day 2 :
Keynote Forum
Mandy J Hill
UT Health Science Center at Houston, USA
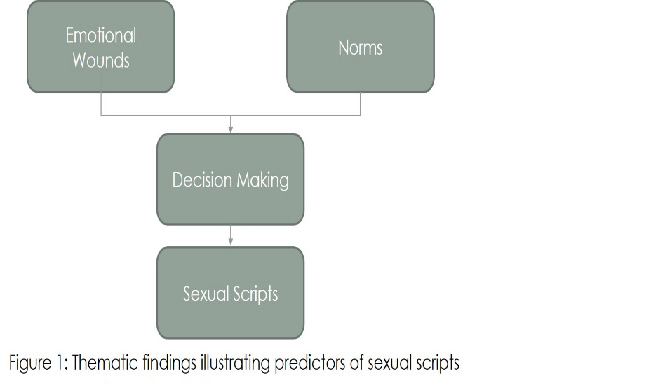
Keynote: Predictors of sexual scripts among young, sexually-active, substance-using African American women
Time : 10:05-10:45

Biography:
Abstract:
Keynote Forum
Sarah Joseph
Senior Scientist, UK
Keynote: Vaccination strategies to maximise Immune Responses using DNA, MVA and adjuvanted gp140
Time : 11:00-11:40

Biography:
Abstract:
- HIV/AIDS, STDs & STIs
Session Introduction
Mohammad Akram Randhawa
Northern Border University, Saudi Arabia
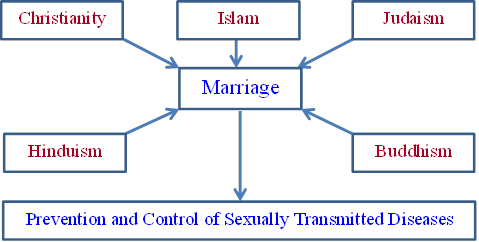
Title: Religions and marriage for the prevention and control of sexually transmitted diseases
Biography:
Abstract:
Gabriela Gore-Gorszewska
Jagiellonian University, Poland
Title: Competent sexual education as a potential STI prevention method. Reflections on ideas from across Europe
Time : 12:10-12:40

Biography:
Abstract:
Joan J Rugemalila
Muhimbili National Hospital, Tanzania
Title: Predictors associated with moderate to severe chronic kidney disease among HIV infected adult patients in Dar es Salaam, Tanzania
Time : 12:40-13:10

Biography:
Abstract:
Vera Ketty
Hospital Matilde Hidalgo de Procel, Ecuador
Title: The high seroreversion of Human Immunodeficiency Virus in vertically exposed infants who received all the care measures to reduce the mother-to-child transmission in Guayaquil, Ecuador
Time : 13:10-13:40
Biography:
Abstract:
- Public Awareness on STDS
Session Introduction
Chloe Chan
New York University, USA
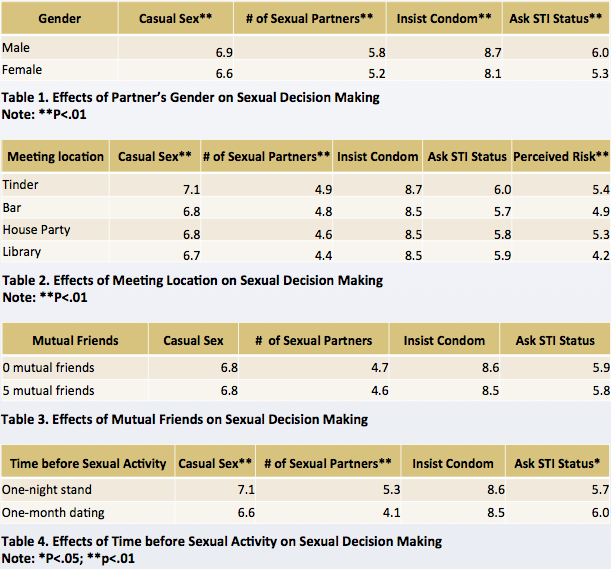
Title: The effects of contextual factors and dating app usage on sexual risk behaviors among young adults
Biography:
Abstract:
Patricia Garcia de Olalla
Public Health Agency of Barcelona, Spain
Title: Does the high prevalence of late presentation of HIV infection persist?
Biography:
Abstract:
Biography:
Abstract:
Gesesew Hailay
Flinders University, Australia
Title: HIV care continuum outcomes: does Ethiopia meet the UNAIDS 90-90-90 targets?

Biography:
Abstract:
- HIV/AIDS, STDs & STIs - testing
Session Introduction
Nagesh Wadgera
BMCRI, India
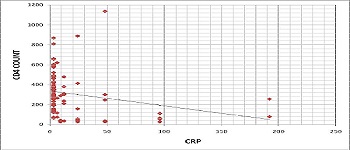
Title: C-reactive protein as an early marker of opportunistic infections in HIV

Biography:
Abstract:
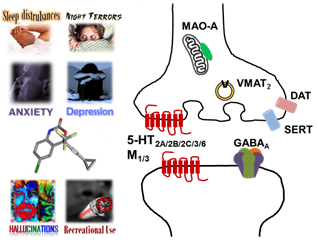
John A Schetz
University of North Texas HSC, USA
Title: Unraveling the complex psychopharmacology associated with the adverse neuropsychiatric side effects and recreational use of HIV-1 antiretroviral drugs

Biography:
Abstract:
Al-Jaroudi D
King Fahad Medical City, Saudi Arabia
Title: Is it important to screen for hepatitis B, C, and HIV in infertile couple?
Biography:
Abstract:
Biography:
Abstract:
Everly Faith Ramos
Philippine General Hospital, Philippines
Title: Typhoid fever presenting as acute psychosis in a patient with HIV infection

Biography:
Everly Faith Ramos is a third year medical resident at the Philippine General Hospital. She obtained her Doctor of Medicine degree from the Uinveristy of the Philippines College of Medicine. She has previously published research studies in the Asian Journal of Biology Education and Acta Madica Philippina.
Abstract:
- Vaccine Development for STDS
